The Power of Early Intervention with ABA Therapy for Autism
In recent years, the conversation around autism has evolved significantly, with a growing emphasis on the importance of early intervention. Among the various approaches, Applied Behavior Analysis (ABA) therapy has gained traction as a highly effective method for supporting individuals on the autism spectrum. At LittleStar, we are committed to providing personalized, impactful care through ABA therapy, making a tangible difference in the lives of children with autism and their families.
The Importance of Early Intervention for Autism
Research consistently highlights the benefits of early intervention for children with autism. A study by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) underscores that early and intensive behavioral interventions can lead to significant improvements in communication, social skills, and adaptive behavior (Early Intervention for Autism). This is echoed by Autism Speaks, which categorizes early intervention as a “highly effective” strategy in its comprehensive overview of autism treatments (Study Finds Early Intervention Highly Effective).
Early intervention with ABA therapy provides structured and systematic support, helping children develop essential skills during critical developmental windows. By addressing challenges early, we can set the stage for more successful outcomes in education and social integration.
Read more about LittleStar’s services for children as young as 18 months.
Personalized Therapy Plans at LittleStar
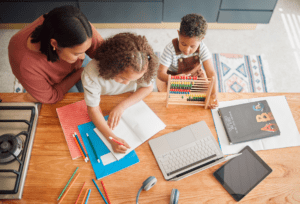
Every child with autism is unique, and their therapy should reflect that. At LittleStar, we pride ourselves on creating individualized ABA therapy plans tailored to each child’s needs, strengths, and goals. Our expert therapists work closely with families to ensure that interventions are both meaningful and measurable.
Our approach is not one-size-fits-all; instead, it is a collaborative process that involves parents, caregivers, and educators. This ensures a comprehensive support system that extends beyond therapy sessions, fostering progress in real-world settings.
Real-Life Transformations

The impact of early intervention with ABA therapy is best illustrated through stories from families who have experienced its benefits firsthand. At LittleStar, we are privileged to witness remarkable transformations in the children we work with.
One parent shared, “Before starting ABA therapy, my child struggled with communication and social interaction. Now, he initiates conversations and engages with peers. The progress has been life-changing for our family.”
Such testimonials underscore the profound impact that tailored ABA therapy can have, not just in improving specific skills but in enhancing overall quality of life.
Addressing Misconceptions about ABA Therapy
Despite its proven effectiveness, ABA therapy is sometimes misunderstood. One common misconception is that ABA is rigid and overly focused on behavior modification. In reality, ABA is a flexible, evidence-based approach that adapts to each individual’s needs, promoting positive reinforcement and skill development.
Another misconception is that ABA is only suitable for young children. While early intervention is crucial, ABA therapy can be beneficial at any age. At LittleStar, we serve individuals of all ages, from toddlers to adults, ensuring continuous support throughout their lives.
Empowering Parents to Make Informed Decisions
Understanding the options available for autism treatment can be overwhelming for parents. At LittleStar, we are dedicated to providing clear, accurate information to empower families in their decision-making process. By demystifying ABA therapy and highlighting its benefits, we aim to build trust and confidence among parents seeking the best care for their children.
Early intervention with ABA therapy represents a powerful tool in supporting the development and well-being of individuals with autism. At LittleStar, our commitment to personalized, compassionate care ensures that each child receives the support they need to thrive. If you are a parent considering ABA therapy, we invite you to reach out to our team and learn more about how we can help your child achieve their full potential. Together, we can make a lasting difference in the lives of children and families affected by autism.
Real Care. Real Advocacy. Real Progress.
LittleStar is a special place for those impacted by autism, with Indiana centers staffed by experienced professionals providing ABA therapy. Our clean, safe facilities are dedicated to improving lives, backed by a non-profit model and a national advisory board of autism experts. We prioritize individual goals, ensure highly qualified team members, and strive to inspire, serve, and guide those affected by autism to a better reality. Our goal is to be a trusted, innovative partner, offering compassionate support and creating new possibilities for individuals with autism throughout their lives.
Follow along with us on Facebook and Instagram as we inspire, serve, and guide all those touched by autism to achieve a better reality.